Leadership challenges in the healthcare industry define how hospitals, clinics, and care systems operate today. From managing costs and adapting to technology to addressing staff retention and patient satisfaction, healthcare leaders face constant pressure to balance care quality with operational efficiency. The industry demands agile decision-makers who can handle policy shifts, workforce shortages, and rapid digital transformation. This article breaks down the core challenges, the skills leaders need, and the strategies that drive strong leadership performance in healthcare organizations.
Key Takeaways
- Healthcare leadership success depends on mastering adaptability, communication, and emotional intelligence.
- The main leadership challenges include balancing care quality, managing new technologies, and sustaining workforce engagement.
- Leadership development and change management in healthcare drive long-term performance and patient outcomes.
Important Healthcare Leadership Skills for Today’s Leaders
The role of a healthcare leader extends far beyond managing departments or budgets. It involves guiding diverse teams, aligning care objectives with financial sustainability, and setting a clear direction amid ongoing change. Strong healthcare leadership skills help organizations stay resilient in unpredictable environments, ensuring patient care remains at the center of every decision.
Leaders must also embrace continuous learning and situational awareness. The ability to read people, interpret data, and act decisively creates a culture of accountability and trust. Every effective healthcare leader knows that progress relies on both technical expertise and emotional intelligence.
Emotional Intelligence and Empathy
Emotional intelligence separates effective leaders from functional managers. In healthcare, you’re constantly dealing with stress, patient emotions, and high-stakes choices. Understanding the emotional context behind every decision helps maintain composure and empathy. Leaders who manage emotions well build stronger relationships with staff, encourage open dialogue, and prevent burnout. Compassion is not a soft skill; it’s a leadership necessity in an industry built on care.
Strategic Communication
Communication is the bridge between policy and practice. Healthcare leaders must translate complex goals into clear, actionable steps for clinical and administrative teams. Strong communicators listen first, address issues quickly, and create feedback systems that improve collaboration. Clarity reduces confusion, supports change management in healthcare, and strengthens trust across all levels of the organization.
Decision-Making Under Pressure
Quick, informed decisions are routine in healthcare. Leaders often act with incomplete data, competing priorities, and ethical dilemmas. The ability to weigh outcomes, rely on trusted experts, and stay calm defines professional maturity. Structured decision frameworks, supported by data analytics and consultation, help leaders stay consistent, fair, and accountable even in tense situations.
Adaptability and Change Leadership
Change is constant in healthcare, from evolving technology to patient expectations. Adaptability allows leaders to pivot without losing focus on care standards. Those who approach change proactively help their teams adjust more smoothly. Change leadership isn’t just about updating systems; it’s about guiding people through uncertainty with confidence and transparency.
7 Common Leadership Challenges in the Healthcare Industry
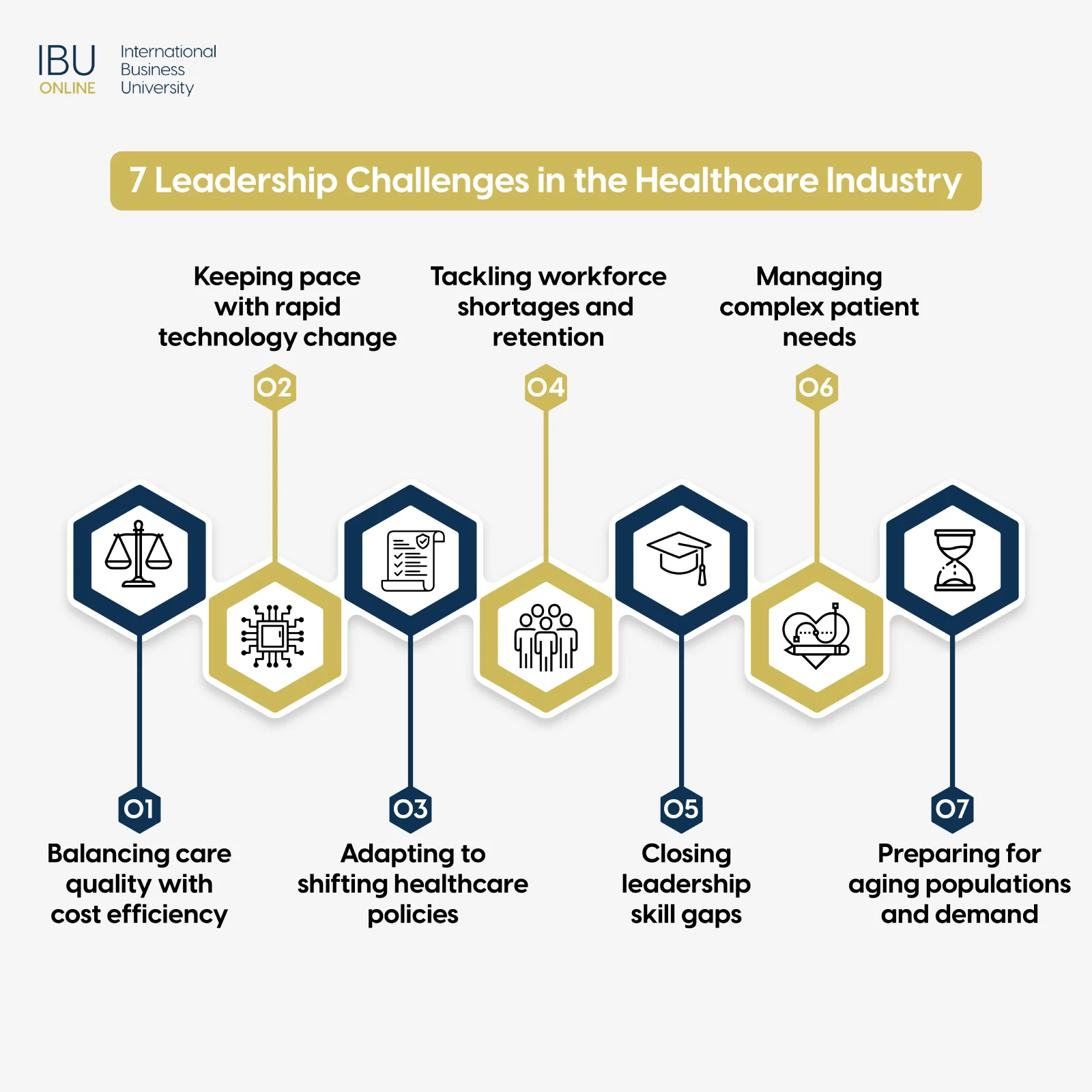
Even the most capable leaders encounter hurdles that test their resilience and strategy. The following challenges outline the main barriers faced in modern healthcare management: balancing financial goals with patient outcomes, adapting to new technologies, handling unpredictable policy shifts, managing workforce retention, closing skill gaps, meeting complex patient needs, and preparing for demographic change. Understanding these challenges helps future healthcare leaders approach their roles with clarity and foresight.
1. Balancing Care Quality with Cost Management
One of the toughest leadership challenges in the healthcare industry is finding equilibrium between delivering exceptional care and managing costs responsibly. Healthcare systems must allocate limited budgets while maintaining high standards of service. Leaders must learn to optimize resources, negotiate vendor agreements, and streamline operations without compromising patient outcomes. Financial discipline paired with clinical awareness enables sustainable healthcare delivery that meets both business and ethical obligations.
2. Managing Rapid Technological Advancements
Technology reshapes how hospitals and clinics function. From electronic health records to AI-based diagnostics, the pace of innovation demands constant adaptation. Leaders must assess which tools genuinely improve outcomes and which add unnecessary complexity. Managing this requires both tech fluency and strategic restraint. Effective leaders introduce technology that enhances efficiency, reduces errors, and supports long-term goals without overwhelming staff or budgets.
3. Navigating Healthcare Policy Uncertainty
Policies shift as governments change priorities, funding structures, and compliance rules. Healthcare leaders must interpret these shifts quickly and align internal practices with evolving regulations. Flexibility and foresight are key. Strong leaders stay informed, maintain legal compliance, and build adaptive frameworks that allow organizations to operate smoothly even during policy transitions. This level of agility ensures the continuity of care and institutional credibility.
4.Workforce Shortages and Staff Retention
Recruiting and retaining skilled professionals remains a critical issue. Many healthcare workers face burnout from workload intensity and emotional strain. Leaders must prioritize well-being, fair scheduling, and supportive environments. Recognizing achievements, offering growth opportunities, and maintaining transparent communication can significantly improve retention. Addressing staff retention in healthcare means investing in people before productivity; it’s the foundation of stable performance.
5. Leadership Skill Gaps and Development
Leadership skill gaps often appear when managers are promoted for technical expertise rather than strategic competence. Hospitals and networks must cultivate structured leadership development in healthcare, training professionals to think system-wide, not just departmentally. Investing in mentorship, cross-functional learning, and executive education strengthens decision quality and collaboration. Building leadership depth prepares organizations for succession and sustained performance.
6. Addressing Complex Patient Needs Holistically
Modern patients expect coordinated, personalized care. Leaders must encourage integrated service models where medical, administrative, and social support teams collaborate. This requires breaking silos and fostering shared accountability for outcomes. When leaders align departments under one patient-centric mission, they create more efficient pathways from diagnosis to recovery, improving satisfaction and clinical results.
7. Preparing for Demographic Shifts and Increased Demand
Aging populations and chronic disease prevalence increase the demand for long-term care and specialized services. Leaders must anticipate these trends and plan resource allocation accordingly. Workforce training, facility upgrades, and digital tools for remote care all become critical. Strategic forecasting ensures organizations can serve evolving community needs without compromising care standards or financial stability.
Build the Leadership Skills the Healthcare Industry Needs
Ready to take the next step in your healthcare management career? Explore IBU’s MBA in Healthcare Management, designed for future industry leaders.
Strategies for Leadership Development in Healthcare Organizations
Healthcare organizations can’t rely on experience alone to produce great leaders. Structured development programs, mentorship opportunities, and continuous learning models keep management aligned with future industry demands. By combining leadership education with real-world application, institutions create adaptive, capable professionals ready to guide teams through complex change.
The first step involves identifying leadership potential early. Healthcare organizations should observe how individuals handle responsibility, communication, and decision-making under pressure. Providing feedback and structured career paths encourages emerging leaders to refine their abilities while staying aligned with organizational goals.
Finally, collaboration across departments plays a vital role. Cross-functional leadership training breaks barriers between clinical and administrative teams, improving trust and coordination. When organizations invest in comprehensive leadership development, they nurture innovation, improve employee morale, and secure better patient outcomes in the long term.
FAQ
Q1: What are the key leadership challenges in the healthcare industry?
They include managing costs, keeping up with technology, handling policy changes, and maintaining staff morale. Leaders also face constant pressure to balance patient care quality with financial constraints. Addressing these challenges demands strong communication and adaptability.
Q2: How does change management impact healthcare leadership?
Change management in healthcare ensures smoother transitions during new initiatives or policy shifts. Leaders who manage change effectively reduce resistance, minimize confusion, and maintain consistent performance. It helps create stability amid constant evolution.
Q3: What essential healthcare leadership skills are needed today?
Leaders must demonstrate emotional intelligence, strategic thinking, communication clarity, and decision-making confidence. These skills help align organizational goals with patient outcomes. Effective leaders inspire collaboration across diverse healthcare teams.
Q4: How can leaders handle staff retention in healthcare?
Retention improves when leaders create supportive cultures, provide training, and recognize contributions. Transparent communication and manageable workloads strengthen loyalty. Employee engagement directly influences the quality of patient care.
Q5: What are common leadership issues in healthcare management?
Common issues include skill shortages, budget limitations, and resistance to change. Leaders often struggle with coordination across departments and ensuring consistent standards. Addressing these issues requires structure, trust, and continuous learning.
Q6: How can leadership development improve healthcare outcomes?
Leadership development equips professionals with strategic, communication, and management tools that improve teamwork and decision quality. Strong leaders drive accountability and innovation. Better leadership leads directly to higher patient satisfaction and operational excellence.
Q7: How do technological advancements affect healthcare leaders?
Technology increases efficiency yet adds complexity to management. Leaders must evaluate tools carefully, train staff effectively, and maintain security compliance. Proper tech adoption transforms operations without overwhelming teams.
Q8: What strategies help overcome workforce shortages in healthcare?
Effective strategies include recruitment partnerships, professional development, and flexible scheduling. Leaders who invest in training and well-being retain talent longer. Consistent workforce planning ensures patient services remain uninterrupted.
Q9: How can leaders manage cost and quality challenges in healthcare?
Leaders balance costs and care by improving process efficiency, reducing waste, and prioritizing preventive care. Collaboration between financial and clinical teams ensures decisions remain ethical and sustainable. Consistent performance tracking helps refine long-term strategies.
Q10: What trends shape future leadership in the healthcare industry?
Data-driven decision-making, virtual care, and patient personalization are redefining leadership priorities. Tomorrow’s leaders must combine empathy with digital literacy. Those who adapt early gain an edge in both efficiency and care quality.
Overcoming Common Leadership Issues in Healthcare Settings
Effective healthcare leadership isn’t about managing tasks; it’s about guiding people through constant transformation. You need the confidence to lead with clarity, the patience to build trust, and the insight to make every decision count. By facing leadership challenges in the healthcare industry head-on, you prepare your team for consistent growth and excellence. The future belongs to leaders who combine strategic thinking with empathy, turning obstacles into measurable progress.
Advance Your Leadership Career in Healthcare
Apply now to join IBU’s industry-aligned MBA in Digital Health and Data Analytics and gain the expertise to lead with confidence in tomorrow’s healthcare sector.
